While Osteoarthritis (OA) is one of the most significant causes of disability worldwide, it has no known cure. A team at the Regenerative Medicine Institute (REMEDI) at NUI Galway, along with European partners, is now seeking to change that.
OA is a painful degenerative disease of the joints. It affects quality of life for people with the condition and those who support them, while also placing a burden on societies and economies around the world.
Having worked with stem cells over recent decades, Mary Murphy, Professor of Regenerative Medicine at REMEDI, is acutely aware of the potential of stem cell-based therapies to repair cartilage, help prevent OA and treat it in patients who already have the condition. Currently, she is co-ordinating and co-leading AutoCRAT, a four-year project funded to the tune of €7.4m under the EU Horizon 2020 programme.
What is AutoCRAT?
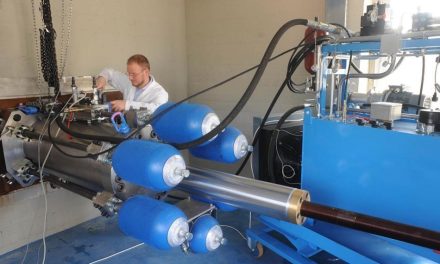
AutoCRAT aims to deliver new cell and cell-derived therapies for osteoarthritis and cartilage repair using sustainable sources of cells by 2024. It also seeks to develop a scalable automated pipeline to enable future production of therapeutic cell-derived products.
While adult stem cell-based therapies are producing good results in early-stage clinical trials, Professor Murphy explains this method of producing cells is high cost and can generate cells that age and die quickly. The AutoCRAT method of deriving the required cells (called mesenchymal stem cells) from pluripotent stem cells can yield many functional cells from a single source.
“We would hope to achieve the capacity for generating enough product to cater to a large population group,” says Professor Murphy.
AutoCRAT stands for Automated Cellular Robot-Assisted Technologies for translation of discovery-led research in Osteoarthritis. The team behind it hopes its work will also have a wider application beyond OA and help to increase the strength of the regenerative medicine sector in general.
A continuous funded research pipeline
The AutoCRAT project builds on the foundations laid in two previous EU-funded projects led by NUI Galway – PurStem and Autostem – and on Professor Murphy’s work with her co-lead and husband Professor Frank Barry (now Professor of Cellular Therapy at NUI Galway) at Osiris Therapeutics in the US, which was the world’s first stem cell company.
Partnering for success
Presenting an innovative research project is critical to secure funding, says Murphy, but she says it’s also vital to connect the right partners for the application with “…people experienced in writing and implementing this type of project, with a history of successful funding from the EU.”
The AutoCRAT project team is made up of nine expert scientific teams in five countries, including specialists in regenerative medicine, OA, preclinical efficacy and safety demonstration, and mesenchymal stem cells (MSC) that are used to treat osteoarthritis. As part of the AutoCRAT project, they look at ways to manufacture these cells for clinical trials addressing regulatory affairs and health economics analysis. The project team includes Irish firm ValitaCell, which focuses on quality control in the manufacturing cycle.
Professor Murphy recommends spending time on building partner relationships. “It’s very important to get to know your partners. Even before our first project, we visited both our German partners, for example. The management within each partner is also important. You need to be able to trust the lead to do what is needed and to have time for the project.”
To keep the complex web of partnerships needed for large research projects working well and on track, Professor Murphy says it’s vital to have a strong project manager. For AutoCRAT, that is Dublin-based Pintail.
“They manage the reporting and there is a lot of it,” she explains. “They make sure it is complete and in on time. In fact, the person we work with has developed considerable knowledge over the years. She can now point out where the science doesn’t make sense!”
Looking to the future
Even with years to run on AutoCRAT, Professor Murphy and her team are looking ahead to how they will further develop their work and how they might fund that progress.
“We could be looking at something like a one-off production unit for patient-derived mesenchymal stem cells (MSC). It would be a customised unit that would allow individual patient product to be generated on a small scale – an example of putting your machine literally next to the patient.”
For this, she says, the team may look to Europe or to Ireland’s Disruptive Technologies Innovation Fund. Either way, the ambition is to see extensive treatment of OA patients with these advanced stem cell therapies as soon as possible, while also helping to improve consistency and efficiency and lower costs in the cell therapy industry.
If you would like advice about accessing Horizon Europe support or further details, please contact horizonsupport@enterprise-ireland.com or visit www.horizoneurope.ie